- MAGNETOM World
- Hot Topics
- MRI in Radiation Therapy
MRI in Radiation TherapyPeer-to-peer exchange of protocols, articles and tips
The MAGNETOM World is the community of Siemens Healthineers MR users worldwide, providing you with relevant clinical information. Here you will find application tips and protocols to optimize your daily work. Lectures and presentations from experts in the field will allow you to be exposed to new ideas and alternative clinical approaches.
Put the advantages of the MAGNETOM World to work for you!
MReadings

MReadings: MR in RT, 11th Edition, ESTRO 2025
Guest Editors: Daniela Thorwarth1 and Daniel Zips2
1 Department of Radiation Oncology, University of Tübingen, Germany
2 Department of Radiation Oncology and Radiotherapy, Charité – Universitätsmedizin Berlin, Germany

MReadings: MR in RT, 10th Edition, ESTRO 2024
Guest Editors: Stephanie Tanadini-Lang and Matthias Guckenberger (Department of Radiation Oncology, University Hospital Zurich (USZ), Switzerland)

MReadings: MR in RT, 9th Edition, ASTRO 2023
Guest Editor: Yue Cao, Departments of Radiation Oncology, Radiology and Biomedical Engineering, University of Michigan, Ann Arbor, MI, USA

MReadings: MR in RT, 8th Edition, ESTRO 2022
Guest Editor: Daniel Low, Dept. of Radiation Oncology, University of California, Los Angeles, CA, USA

MReadings: MR in RT, 7th Edition, 2021
Guest Editor:
Christian Kirisits, Department of Radiation Oncology, Comprehensive Cancer
Center, Medical University of Vienna, Austria

MReadings: MR in RT, 6th Edition, ESTRO 2020
Guest Editor: Caroline Chung, The University of Texas MD Anderson Cancer Center, Houston, TX, USA

MReadings: MR in RT, 5th Edition, ESTRO 2019
Guest Editor: Jürgen Debus, University Hospital Heidelberg, Germany

MReadings: MR in RT, 4th Edition, ESTRO 2018
Guest Editor: Paul Keall, Sydney Medical School, University of Sydney, Australia

MReadings: MR in RT, 3rd Edition, ESTRO 2017
Guest Editor: David Jaffray, Princess Margaret Cancer Centre, Toronto, Canada

MReadings: MR in RT, Second Extended Edition
Protocols / QA

Commissioning and Quality Assurance (QA) for MAGNETOM systems in radiation therapy
This QA cookbook is a guide for medical physicists and technologists on how you can perform quality assurance procedures for Radiation Therapy planning on your MAGNETOM scanner. This guide is not intended to replace or supersede the user manual or instructions for use for the MAGNETOM MR scanner but act simply as a suggested supplement to meet specific QA needs for radiotherapy.

ACR Phantom QA Test
Download the protocol for carrying out the ACR phantom QA test on your 1.5 or 3T MAGNETOM system.
Please refer to the procedure described in Appendix 3 of the guide Commissioning and Quality Assurance (QA) for MAGNETOM systems in radiation therapy

Commissioning and Implementing a Quality Assurance Program for Dedicated Radiation Oncology MRI Scanners
Éric Poulin, et al. (Université Laval, Québec, Canada)
Protocols for MR-integrated Workflows in Radiation Therapy
MAGNETOM World is the link allowing MAGNETOM users worldwide to capitalize on the advantages of belonging to this community.
On this page renowned experts share their optimized MR protocols and we would like to express our sincere gratitude to everyone who contributes to this valuable exchange.
MAGNETOM Skyra 3T protocols
Protocol courtesy of Kate Skehan, et al.; Calvary Mater Hospital, Newcastle, NSW, Australia
As published in: Richardson M, Skehan K, Wilton L, Sams J, Samuels J, Goodwin J, Greer P, Sridharan S, Martin J. Visualising the urethra for prostate radiotherapy planning. J Med Radiat Sci. 2021 Sep;68(3):282-288. doi: 10.1002/jmrs.485.

Contact
Kate Skehan, B.Med.Rad.Sc.
Senior MRI Radiographer
Department of Radiation Oncology
Calvary Mater Hospital
Newcastle, NSW 2298
Australia
Tel.: (02) 4014 3166
kate.skehan@calvarymater.org.au
Courtesy of Leah Best, et al., Calvary Mater Hospital Newcastle, Newcastle, NSW, Australia
- Liver .exar1 (binary/octet-stream) 0.79 MB
- Upload Liver .exar1 to teamplay Protocols
- Liver .exar1-journal (binary/octet-stream) 0.13 MB
- Upload Liver .exar1-journal to teamplay Protocols
- Prostate .exar1 (binary/octet-stream) 0.41 MB
- Upload Prostate .exar1 to teamplay Protocols
- Spine .exar1 (binary/octet-stream) 0.24 MB
- Upload Spine .exar1 to teamplay Protocols

Contact
Leah Best, MSc
Calvary Mater Hospital
Newcastle, Newcastle,
NSW, Australia
leah.best@hnehealth.nsw.gov.au
MAGNETOM Aera 1.5T protocols
Courtesy of Cynthia Eccles, Helen McNair, Trina Herbert, and Shree Bhide,
The Royal Marsden NHS Foundation Trust, Sutton, UK

Contact
Trina Herbert
The Royal Marsden
NHS Foundation Trust,
Sutton, UK
trina.herbert@rmh.nhs.uk
MAGNETOM Verio 3T protocols
Courtesy of Eric Paulson, Ph.D., Medical College of Wisconsin, Milwaukee, USA
- Head and Neck .edx (edx) 0.1 MB
- Upload Head and Neck .edx to teamplay
- Esophagus .edx (edx) 0.1 MB
- Upload Esophagus .edx to teamplay Protocols
- Pancreas .edx (edx) 0.1 MB
- Upload Pancreas .edx to teamplay Protocols
- Liver .edx (edx) 0.1 MB
- Upload Liver .edx to teamplay Protocols
- Brachy Cervix .edx (edx) 0.1 MB
- Upload Brachy Cervix .edx to teamplay Protocols
- Prostate .edx (edx) 0.1 MB
- Upload Prostate .edx to teamplay Protocols

Contact
Eric Paulson, Ph.D., DABR
Assistant Professor and Senior Medical Physicist
Radiation Oncology, Radiology, and Biophysics
Medical College of Wisconsin
Radiation Oncology
8701 Watertown Plank Road
Milwaukee, WI 53223
USA
epaulson@mcw.edu
MAGNETOM Skyra 3T protocols
Courtesy of Robba Rai, Liverpool and Macarthur Cancer Therapy Centre and Gary Liney, Ph.D., Ingham Institute for Applied Medical Research, Sydney, Australia
- Brain .exar1 (binary/octet-stream) 2.67 MB
- Upload Brain .exar1 to teamplay Protocols
- Head and Neck .exar1 (binary/octet-stream) 1.94 MB
- Upload Head and Neck .exar1 to teamplay Protocols
- Extremities .exar1 (binary/octet-stream) 0.25 MB
- Upload Extremities .exar1 to teamplay Protocols
- Lung .exar1 (binary/octet-stream) 1.55 MB
- Upload Lung .exar1 to teamplay Protocols
- Sarcoma .exar1 (binary/octet-stream) 0.24 MB
- Upload Sarcoma .exar1 to teamplay Protocols
- TimCT .exar1 (binary/octet-stream) 0.31 MB
- Upload TimCT .exar1 to teamplay Protocols

Contact
Associate Professor Gary Liney (UNSW)
Hon Principal Fellow, University of Wollongong Ingham Institute for Applied Medical Research & Radiation Oncology
Liverpool Hospital, 1 Campbell Street
Liverpool NSW 2170
Australia
Phone: +61 2 8738 9221
gary.liney@sswahs.nsw.gov.au

Robba Rai
Senior MRI Radiographer
Liverpool Cancer Therapy Centre
robba.rai@sswahs.nsw.gov.au
MAGNETOM Aera 1.5T protocols
Courtesy of Maja Sohlin, Ph.D., Sahlgrenska University Hospital, Gothenburg, Sweden
- Brain .exar1 (binary/octet-stream) 0.22 MB
- Upload Brain .exar1 to teamplay Protocols
- Brain Stereo .exar1 (binary/octet-stream) 0.32 MB
- Upload Brain Stereo .exar1 to teamplay Protocols
- Head Schwanoma .exar1 (binary/octet-stream) 0.2 MB
- Upload Head Schwanoma .exar1 to teamplay Protocols
- Head Schwanoma .exar1-journal (binary/octet-stream) 0.13 MB
- Upload Head Schwanoma .exar1-journal to teamplay Protocols
- Head and Neck .exar1 (binary/octet-stream) 0.24 MB
- Upload Head and Neck .exar1 to teamplay Protocols
- Prostate .exar1 (binary/octet-stream) 0.37 MB
- Upload Prostate .exar1 to teamplay Protocols
- Cervix Brachy .exar1 (binary/octet-stream) 0.66 MB
- Upload Cervix Brachy .exar1 to teamplay Protocols

Contact
Maja Sohlin, Ph.D.
Medical Physicist
Sahlgrenska University Hospital
Medical Physics and Biomedical Engineering
Bruna stråket 13
413 45 Gothenburg
Sweden
maja.sohlin@vgregion.se
MAGNETOM Skyra 3T protocols
Courtesy of Yue Cao, Ph.D., University of Michigan, Ann Arbor, MI, USA

Contact
Yue Cao, Ph.D.
Physics division
Department of Radiation Oncology
University of Michigan
Ann Arbor, MI
USA
yuecao@med.umich.edu
MAGNETOM Aera 1.5T protocols
Courtesy of Cynthia Ménard, M.D., FRCPC and David Roberge, M.D., FRCPC, Centre hospitalier de l’Université Montréal (CHUM), Montréal, QC, Canada

Contact
Cynthia Ménard, M.D., FRCPC
Centre hospitalier de l’Université de Montréal
Cancer Clinical Research Unit (CCRU)
Princess Margaret Cancer Centre
1560 Sherbrooke St E
Montréal, QC
Canada, H2L 4M1
cynthia.menard@umontreal.ca
Application Tips
The Application Tips are a platform to contribute and to continuously expand your knowledge. Share your experience with other MAGNETOM users and perfect your ability to exploit the full potential of your MAGNETOM system.

Application of TGSE-BLADE DWI in Radiotherapy Treatment Planning
Yutaka Kato, et al. (Dept. of Radiological Technology, Nagoya University Hospital, Nagoya, Japan)

Signal-Based Motion Management in Abdominal MRI for Radiotherapy Planning
Terumasa Takemaru, et al. (Global Education Specialist MR, Siemens Healthineers, Erlangen, Germany)

Magnets, Spins, and Resonances
An introduction to the basics of Magnetic Resonance.

Magnets, Flows, and Artifacts
Techniques and Applications of Magnetic Resonance.

MR Glossary
A Dictionary of Magnetic Resonance.

Bring-Your-Own-Phantom (BYOP): A Flexible Stand-Alone Distortion Analysis Prototype
Niranjan Venugopal, M.Sc., Ph.D., MCCPM; et al. (University of Manitoba, CancerCare Manitoba, Winnipeg, Canada)
In order to optimize Radiotherapy Planning for MRI, care must be taken to reduce geometric distortions as much as possible. The myExam RT Assist1 is designed with optimized protocols for Radiotherapy planning and is one tool to help mitigate distortions. For users who have created their own sequences or customized certain ones, other tools may help to reduce geometric distortions. For those users, there may be several specific parameters that need to be checked for each different sequence type. The Siemens Healthineers Generic View AddIn allows you to create a bespoke template for your individual needs enabling you to quickly move the AddIn from one sequence to the next to efficiently check your chosen parameters. Three examples are given for RESOLVE, TSE, and SPACE. E.g. where a T2 sequence has been optimized but a T1 is needed. The AddIn can be moved to the new sequence and the parameters checked prior to scanning.

Lynn Doy, DCR(R) MSc; et al. (North West Cancer Centre, Altnagelvin Area Hospital, Londonderry, Northern Ireland)

Synthetic CT Generation for the Pelvic Region Based on Dixon-MR Sequences: Workflow, Dosimetric Quality and Daily Patient Positioning
Daniela Thorwarth, et al., University Hospital Tübingen, Germany

Optimizing MRI sequences and images for MRI-based stereotactic radiosurgery treatment planning
Ali Fatemi, Ph.D. et al., University of Mississippi Medical Center, Jackson, MS, USA

Machine-specific MRI quality control procedures for stereotactic radiosurgery treatment planning
Ali Fatemi, Ph.D. et al., University of Mississippi Medical Center, Jackson, MS, USA

Whole-body MRI at 1.5T – step-by-step
Will McGuire, Anwar Padhanin et al., Paul Strickland Scanner Centre, Mount Vernon Hospital, Northwood, Middlesex, UK

How-I-Do-It: Comprehensive RT-Specific QA for MRI Simulation
Eric Paulson, Ph.D., DABR, Medical College of Wisconsin, Radiation Oncology, Milwaukee, WI, USA

MRI Geometric Distoriton QA. Using the ACR MRI Accrediation Phantom
This document is a brief instruction on how the ACR (American College of Radiology) accreditation phantom can be used to evaluate geometric distortions in MRI for quality assurance (QA) purposes.

Evaluation of the CIVCO Indexed Patient Position System (IPPS) MRI-Overlay for Positioning and Immobilization of Radiotherapy Patients
Thomas Koch, Ph.D., et al., Klinik und Praxis für Strahlentherapie und Radioonkologie, Sozialstiftung Bamberg, Germany

MAGNETOM Combi Suite Radiation Therapy. Combining MRI Intelligence and Therapeutic Expertise
Annemarie Hausotte, Ph.D., Siemens Healthineers, Erlangen, Germany
MAGNETOM Skyra as an MR Sim
Gary Liney, Liverpool Cancer Therapy Centre, Sydney, Australia
Insights
In this section, you will learn more about the functionality and advantages of MRI and its special use in Radiation Therapy (RT).
Magnetic Resonance Imaging for Radiation Therapy
Why MRI in RT? The clinical motivation
Magnetic Resonance Imaging for Radiation Therapy
What is MRI and how does it work? Part 1
Magnetic Resonance Imaging for Radiation Therapy
What is MRI What is MRI and how does it work? Part 2
Magnetic Resonance Imaging for Radiation Therapy
Challenges in MRI in RT
Magnetic Resonance Imaging for Radiation Therapy
Solving the challenges of MR in RT
Signla, noise, distortion - 1.5T vs. 3T
Magnetic Resonance Imaging for Radiation Therapy
Solving the challenges of MR in RT
Gradients, RF system and coils
Magnetic Resonance Imaging for Radiation Therapy
Solving the challenges of MR in RT
Sequences, incl. DWI, Perfusion, Spectroscopy
Magnetic Resonance Imaging for Radiation Therapy
Solving the challenges of MR in RT
QA for MR, MR Safety, MR Installation

Magnets, Spins, and Resonances
An introduction to the basics of Magnetic Resonance.

Magnets, Flows, and Artifacts
Techniques and Applications of Magnetic Resonance.

MR Glossary
A Dictionary of Magnetic Resonance.
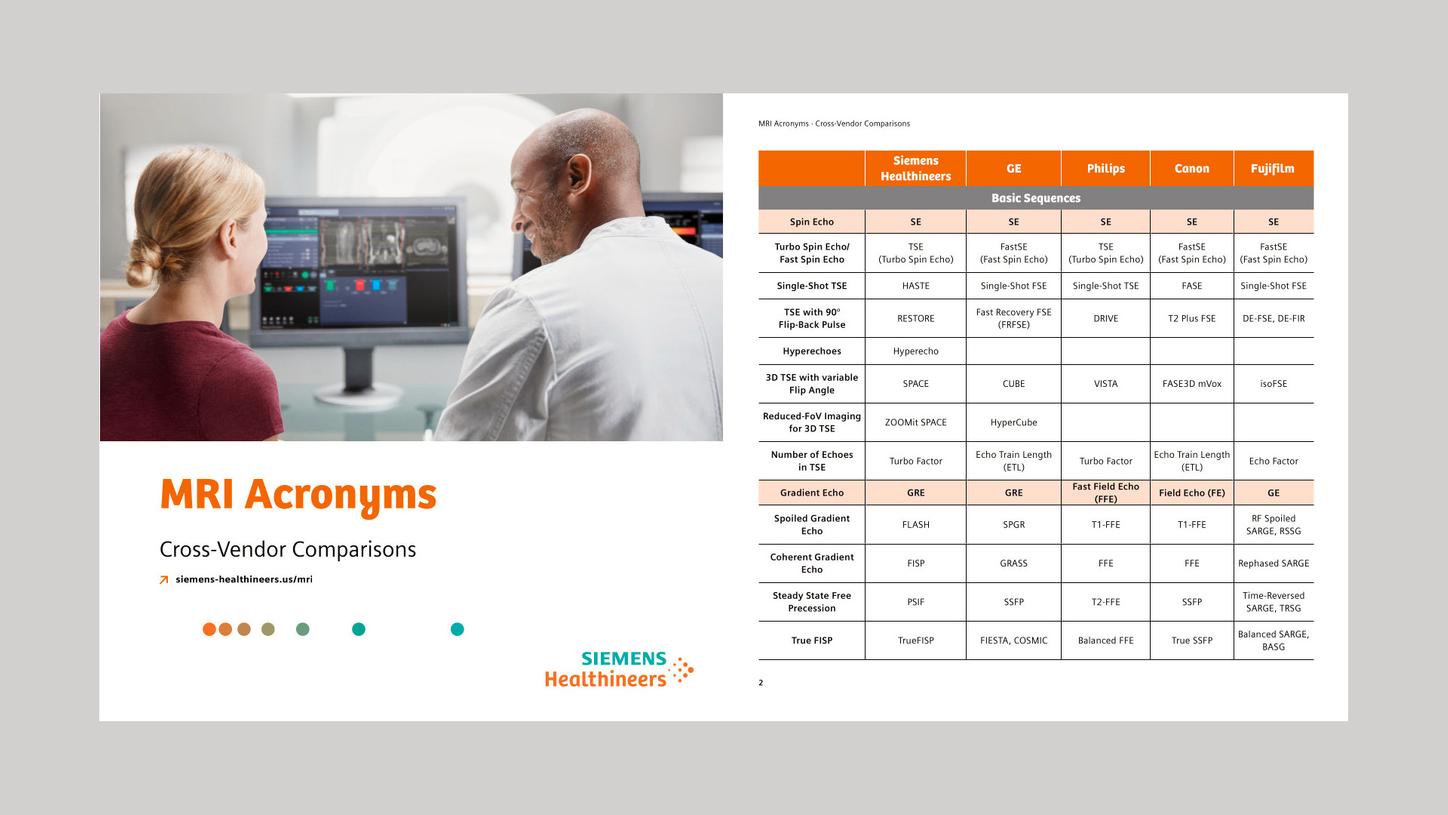
MRI Acronyms
MRI Acronyms is a cross-vendor comparison of sequences and techniques. It is helpful when switching from one vendor to another or when colleagues with different system experience work together.

30 years of MRI at Siemens
A success story.
Articles & Case Studies
Following the rapid adoption of MRI in radiation therapy, Siemens Healthineers has developed tailored solutions that also address those departments that have traditionally used CT imaging alone. On these pages of the MAGNETOM World we aim to increase peer-to-peer exchange of practices and to demonstrate how MAGNETOM users around the world are tackling the challenges posed by the introduction of MRI in the radiotherapy routine.

Exploring the Role of MRI in Lattice Radiotherapy
Chun-yu He, Ph.D.; Bing Li, Ph.D.; et al. (Department of Radiation Oncology, the Affiliated Cancer Hospital of Zhengzhou University & Henan Cancer Hospital, Zhengzhou, Henan, China)

MRI and Radiotherapy: A Transformative Alliance in Modern Oncology Seeking the Best Results with the Best Quality of Life
Dr. Federico Bakal I. (Bradford Hill Clinical Research, Santiago, Chile)

Clinical Implementation of 0.55T MRI Simulation for Stereotactic Radiotherapy Using the MAGNETOM Free.Max RT Edition
Joshua Kim, Ph.D.; Kundan Thind, Ph.D.; et al. (Department of Radiation Oncology, Henry Ford Health, Detroit, MI, USA)

MAGNETOM Free.Max Simulator: First Impressions
Aaron M. Allen, M.D.; et al. (Department of Radiation Oncology, Helmsley Cancer Center, Shaare Zedek Hospital, Jerusalem, Israel)

Integrating MRI into Radiotherapy: Insights from Clinical Implementation of an MRI-Guided Workflow for Prostate Cancer
Philipp Schubert, M.D.; Florian Putz, M.D.; et al. (Dept. of Radiation Oncology, Universitätsklinikum Erlangen, Germany)

Integrating MRI into Radiotherapy: Insights from Clinical Implementation of an MRI-Guided Workflow for Prostate Cancer
Philipp Schubert, M.D.; Florian Putz, M.D.; et al. (Dept. of Radiation Oncology, Universitätsklinikum Erlangen, Germany)

Enhancing Precision in Radiation Therapy by Integrating MRI into Treatment Planning
Sushil Beriwal, M.D.; Deepak Khuntia, M.D. (Varian, a Siemens Healthineers Company)

Implementing MR-Only Workflows for Radiation Therapy Planning: Experiences from Clinical Practice
Krzysztof Ślosarek, Ph.D.; et al. (Radiotherapy Planning Department, National Institute of Oncology, Maria Skłodowska-Curie National Research Institute, Gliwice Branch, Poland)

Bringing Spectroscopic MRI Closer to Clinical Adoption: Results Guiding Radiation Treatment of High-Grade Gliomas
Hyunsuk Shim, PhD; et al. (Emory University, Atlanta, GA, USA)

Combining CT-Based Online Adaptive Radiotherapy with Offline MR Guidance: The Modular Adaptive Radiotherapy System (MARS)
Fabian Weykamp, M.D.; et al. (Heidelberg University Hospital; DKFZ, Heidelberg, Germany)

Biologically Targeted Radiation Therapy (BiRT): From Concept to Clinical Translation
Annette Haworth, Ph.D.; et al. (Institute of Medical Physics, Faculty of Science, The University of Sydney, Australia)

A Decade of Transformative Evolution: The MAGNETOM World RT Community
Elena Nioutsikou, Ph.D. (Varian, a Siemens Healthineers Company, Forchheim, Germany)

From CT to MR: Clinical Experience and Evaluation of MR-Only Simulation for Radiotherapy Planning of Brain Lesions
Jeffrey C.F. Lui, M.Sc. (Department of Clinical Oncology, Queen Elizabeth Hospital, Hong Kong)

Brachytherapy Treatment Planning for Cervical Cancer Patients Using a Lower Magnetic Field MR Scanner
Tibor Major, PhD; et al. (Radiotherapy Centre, National Institute of Oncology, Budapest, Hungary)

4D-MRI for Treatment Planning of Liver Tumors
Jessica Scholey, Ph.D., DABR; et al. (Department of Radiation Oncology, University of California, San Francisco, CA, USA)

Editorial Comment
Daniel Low, Ph.D., FAAPM, FASTRO (University of California at Los Angeles (UCLA), USA)

PETRA Sequence for Catheter Detection in Interstitial High-Dose-Rate (HDR) Brachytherapy
Evangelia Kaza, Ph.D.; Ivan Buzurovic, Ph.D. (Brigham and Women’s Hospital, Dana-Farber Cancer Institute, Harvard Medical School, Boston, MA, USA)

The Application and Utility of Radiotherapy Planning MRI at the Cancer Institute Hospital of JFCR
Yasuo Yoshioka, M.D., Ph.D. (Cancer Institute Hospital of the Japanese Foundation for Cancer Research, Tokyo, Japan)

Christian Kirisits (Dept. of Radiation Oncology, Comprehensive Cancer Center, Medical University of Vienna, Austria)

Rhydian Powell, et al. (North West Cancer Centre, Altnagelvin Area Hospital, Londonderry, Northern Ireland)

MRI-only Based External Beam Radiation Therapy of Prostate Cancer
Jean-François Cabana, M.Sc.; et al. (Centre régional intégré de cancérologie de Chaudière-Appalaches (CRIC), Lévis, QC, Canada)

Optimization of MR Acquisition for Brain Irradiation
Christoph Bert, Ph.D.; et al. (Dept. of Radiation Oncology, University Hospital Erlangen, Germany)

Clinical Evaluation of a Receiver Coil Custom Designed for MR Simulation of Immobilized Patients
James M Balter, Ph.D.; et al. (Dept. of Radiation Oncology, University of Michigan, Ann Arbor, MI, USA)

Implementation of a Process for Radiosurgery Incorporating Functional MRI
Ricardo Ruggeri, MSc.; et al. (Medical physics department, Leben Salud, Patagonia, Argentina)

Clinical Implementation of MR-Guided RT for Prostate Cancer in Halcyon-System
Mandy Zimmermann, et al., Radiologische Allianz, Hamburg, Germany

Advancing MR to Fulfil its Role in Oncology: Time to Finish the Privot from Adjunctive to Essential
Caroline Chung, The University of Texas MD Anderson Cancer Center, Houston, TX, USA

Clinical Implementation and Evaluation of MR-only Radiotherapy Planning for Brain Tumors
David Roberge and Jean-Charles Côté, Centre Hospitalier de l’Université de Montréal, Canada

MR Imaging in Radiosurgery for Trigeminal Neuralgia
Krzysztof Ślosarek et al.,Maria Sklodowska-Curie National Research Institute of Oncology, Gliwice, Poland

MRI for Target Delineation in Radiotherapy – an Overview of Treatment Indications
Florian Putz, et al., Friedrich-Alexander University Erlangen-Nuremberg, Erlangen, Germany

Post Treatment MR of Prostate Cancer
Silvia D. Chang, et al., Vancouver General Hospital and BC Cancer, Vancouver, BC, Canada

Editorial Comment: MR-guided Radiotherapy: the Beginning of a New Era?
Jürgen Debus, University Hospital Heidelberg, Germany

10 Years of Clinical Experience of MRI in Radiotherapy Treatment Planning: The Newcastle upon Tyne Story
Hazel McCallum, et al., Newcastle upon Tyne Hospitals NHS Foundation Trust, Newcastle upon Tyne, UK

The Importance of Collaboration between Clinical Radiology and Radiation Oncology in the Era of Precision Radiation Therapy
Amish Lakhani, et al., Mount Vernon Hospital, Northwood, Middlesex, UK

Synthetic CT Generation for the Pelvic Region Based on Dixon-MR Sequences: Workflow, Dosimetric Quality and Daily Patient Positioning
Daniela Thorwarth, et al., University Hospital Tübingen, Germany

Editorial Comment: MRI and cancer radiotherapy
Paul Keall, University of Sydney, Australia

Replacement of a CT-simulator with an MRI-simulator within a radiation oncology department
Peter Greer et al., Calvary Mater Newcastle, Newcastle, Australia

MRI for prostate and gynecological brachytherapy is here to stay
Firas Mourtada, Ph.D. et al., Helen F. Graham Cancer Center & Research Institute, Newark, USA

MR-only guided proton therapy: advances, future perspectives and challenges
R.J.H. Borra, M.D., Ph.D. et al., University Medical Center Groningen, Groningen, The Netherlands

MR-simulation for radiotherapy treatment planning of head and neck cancer using 3T MAGNETOM Vida
Daniela Thorwarth et al., University of Tübingen, Germany

Dynamic 2D magnetic resonance imaging for assessment of larynx motion in early glottic cancer radiotherapy
Houda Bahig, M.D. et al., Centre Hospitalier de l’Université de Montréal, Montreal, QC, Canada

Improved therapy response assessment in metastatic brain tumors
Kyrre Eeg Emblem, Ph.D. et al., Oslo University Hospital, Oslo, Norway

Spectroscopic MRI for dose-escalated radiation therapy
Hyunsuk Shim, Ph.D. et al., Winship Cancer Institute of Emory University, Atlanta, GA, USA

MyoMap quantification of myocardial toxicity following concurrent chemoradiotherapy for esophageal carcinoma
Gary Liney et al., Liverpool Cancer Therapy Centre, Sydney, Australia

First experience of 4D-MRI for abdominal radiotherapy planning
Andrew Oar et al., Liverpool and Macarthur Cancer Therapy Centre, Sydney, Australia

Quantitative WB-MRI with ADC histogram analysis for response assessment in diffuse bone disease
Anwar R. Padhani et al., Paul Strickland Scanner Centre, Northwood, Middlesex, United Kingdom

Diffusion and perfusion MR parameters to assess preoperative short course radiotherapy response in locally advanced rectal cancer: a comparative explorative study among parameters derived from standardized index of shape DCE-MRI, intravoxel incoherent motion and diffusion kurtosis imaging
Biagio Pecori et al., Istituto Nazionale Tumori (IRCCS), Fondazione G. Pascale, Naples, Italy

Editorial Comment: MRI in Radiation Therapy
David A. Jaffray, Princess Margaret Cancer Centre, Toronto, Canada

4D-MRI Sequence for Radiotherapy Application: Validation of a Retrospective Method on a Motion Phantom
Soléakhéna Ken, Ph.D. et al., Institut Universitaire du Cancer de Toulouse Oncopôle, Toulouse, France

MRI in Head and Neck Radiotherapy Planning
Houda Bahig, M.D. et al., Centre Hospitalier de l’Université de Montréal, Montreal, QC, Canada

Optimizing Fiducial Markers for MRI-based Radiotherapy
Ingemar Näslund, M.D., Ph.D. et al., Karolinska Institutet, Stockholm, Sweden

Performing Gynecologic Brachytherapy in the Medical Innovation Technical Expert Center
Lia Verhoef et al., Department of Radiation Oncology, Radboud University Medical Center, Nijmegen, Netherlands

Early Measures of Perfusion and Diffusion Changes Using a Standardized Analysis Platform Evaluated in Brain Metastases Treated with Stereotactic Radiosurgery
Catherine Coolens, Ph.D. et al., Princess Margaret Cancer Centre and University Health Network, University of Toronto, Toronto, ON, Canada

Integration of Diffusion-Weighted Imaging / Diffusion Tensor Imaging into Radiation Therapy Treatment Planning of Brain Tumors
Tong Zhu, Ph.D. et al., University of North Carolina at Chapel Hill, NC, USA

Initial Clinical Experience Utilizing 4D-MRI for Radiation Treatment Planning
Eric S. Paulson, Ph.D., DABR et al., Medical College of Wisconsin, Milwaukee, WI, USA

Metastatic Prostate Cancer in Practice – the MET-RADS-P Imaging Response System Using Whole-body MRI
Prof. Anwar R. Padhani, MB, BS, FRCP, FRCR et al., Paul Strickland Scanner Centre, Northwood, Middlesex, UK

Observing Endocrine Therapy Resistance in Metastatic Breast Cancer with Whole-body MRI
Anwar R. Padhani et al., Paul Strickland Scanner Centre, Northwood, Middlesex, UK

Whole-body Diffusion-weighted MR Image Analysis with syngo.via Frontier MR Total Tumor Load
Robert Grimm, Ph.D. et al., Siemens Healthineers, Erlangen, Germany

Whole-body MR Image Reading and Bone Assessment with syngo.via Frontier MR Bone Scan
Matthias Fenchel, Ph.D. et al., Siemens Healthineers, Erlangen, Germany

Magnet Homogeneity and Shimming
Mathias Blasche, MS et al., Siemens Healthineers, Erlangen, Germany

Radiotherapy Planning Using MRI
Maria A. Schmidt, Ph.D. et al., Royal Marsden NHS Foundation Trust and Institute of Cancer Research, Sutton, UK

Benefits of Time-Correlated and Breath-Triggered MR
Soléakhéna Ken, Ph.D. et al., Institut Universitaire du Cancer de Toulouse Oncopôle, Toulouse, France

Comprehensive RT-Specific QA for MRI Simulation
Eric Paulson, Ph.D., DABR, Medical College of Wisconsin, Milwaukee, WI, USA

Management of MRI Spatial Accuracy for Radiation Therapy
Teo Stanescu, PhD et al., Princess Margaret Cancer Centre, Toronto, ON, Canada

MRI in Clinical Radiation Oncology: Dosimetry and Patient-Specific Plan Verification
Niko Papanikolaou, Ph.D. et al., University of Texas Health Science Center, San Antonio, Texas, USA

MR-guided Gynecological High Dose Rate (HDR) Brachytherapy
Joann I. Prisciandaro, Ph.D. et al., University of Michigan, Ann Arbor, MI, USA

Multi-parametric MRI at 3 Tesla for Prediction of Treatment Response in Rectal Cancer
Dr. Trang Pham et al., Liverpool Cancer Therapy Centre, Sydney, Australia

Significant Benefit of Optimized 3D SPACE Sequences in Radiation Therapy Treatment
Maja Sohlin, Ph.D. et al., Sahlgrenska University Hospital, Gothenburg, Sweden

The Potential Role of Ultrashort Echo Time Sequences in MRI Guided Radiotherapy
Gary Liney et al., Liverpool Cancer Therapy Centre, Liverpool Hospital, Sydney, Australia

4D-MRI: Future of Radiotherapy of Moving Targets?
Antony John Lomax et al., Center for Proton Therapy (CPT), Paul Scherrer Institut, Villigen PSI, Switzerland

Development of MR-only Planning for Prostate Radiation Therapy Using Synthetic CT
Peter Greer, Ph.D. et al., Calvary Mater Newcastle, Newcastle, New South Wales, Australia

myExam RT Assist1
Gregor Thörmer, Ph.D. et al., Siemens Healthineers, Erlangen, Germany

Anatomical and Functional MRI for Radiotherapy Planning of Head and Neck Cancers
Maria A. Schmidt, Ph.D. et al., Cancer Imaging Centre, Royal Marsden NHS Foundation Trust and Institute of Cancer Research, Sutton, UK

syngo.via RT Image Suite: Empower Radiation Therapy with MRI Information
Elena Nioutsikou, Siemens Healthineers, Forchheim, Germany

Technical Aspects of MR-only Radiotherapy
Tufve Nyholm et al., Umeå University, Sweden

A Dedicated MRI Scanner for Radiotherapy Planning: Early Experiences
Gary Liney, Liverpool Cancer Therapy Centre, Liverpool Hospital, Sydney, Australia

MR-guided Gynecological High Dose Rate (HDR) Brachytherapy
Joann I. Prisciandaro, Ph.D. et al., Department of Radiation Oncology, University of Michigan, Ann Arbor, MI, USA

Clinical Application of Diffusion Tensor Imaging in Radiation Planning for Brain Tumors
Jatta Berberat, Ph.D. et al., Radiation Oncology, Canton Hospital, Aarau, Switzerland

Optimizing MRI for Radiation Oncology: Initial Investigations
James M. Balter, Ph.D., FAAPM et al., Department of Radiation Oncology, University of Michigan, Ann Arbor, MI, USA

Case Report: Functional, Volumetric, Treatment Response Assessment Using MR OncoTreat
Ihab R. Kamel, M.D., Ph.D. et al., The Russell H. Morgan Department of Radiology and Radiological Science, The Johns Hopkins Hospital, Baltimore, MD, USA
Talks & Videos
From technology to clinical applications, here you find talks that allow you to continuously expand your knowledge and perfect the ability to exploit the full potential of your investment, your MAGNETOM System.
BrICS - spectroscopic MRI for dose-escalated RT
Glioblastoma is the most common primary adult brain tumor in the US, with over 10,000 cases diagnosed each year. The current standard of care for these patients is the removal of as much tumor as possible via neurosurgery followed by radiation therapy and concurrent chemotherapy. Despite aggressive treatment, glioblastomas continue to progress and recur within months of treatment, and median survival remains poor at 15 months. Thus, better approaches are needed for targeting both enhancing and non-enhancing tumor to maximize the benefits of high dose radiation.
The Brain Imaging Collaboration Suite (BrICS)4 is a web-based software designed specifically to integrate spectroscopic MRI with clinical imaging, enabling physicians to evaluate metabolic activity, review underlying spectra on a voxel-basis, and delineate target volumes for RT planning. By making whole-brain spectroscopic MRI more accessible for clinical decision-making and treatment decisions through an easy-to-use, collaborative web application, we can improve patient outcomes and drive future of state-of-the-art glioblastoma care.
Further Reading

Spectroscopic MRI for dose-escalated radiation therapy
Hyunsuk Shim, Ph.D. et al., Department of Radiation Oncology, Winship Cancer Institute of Emory University, Atlanta, GA, USA

Clinical Talks
The Integration of MRI in Radiation Therapy: the Power of Multidisciplinary Collaboration
Collaboration between Radiology and Radiation Oncology for MR-guided Radiotherapy1
Hersh Chandarana (New York University, New York, NY, USA)
Implementing a Magnet Dedicated to Planning Radiotherapy Treatments
David Roberge (Centre Hospitalier de l'Université de Montréal, Canada)
MRI in Radiation Oncology. See what you treat - treat what you see1,2
Juergen Debus (University Hospital Heidelberg, Germany)
Collaboration between Radiology and Radiation Oncology for MR-guided Radiotherapy1
Hersh Chandarana (New York University, New York, NY, USA)
Implementing a Magnet Dedicated to Planning Radiotherapy Treatments
David Roberge (Centre Hospitalier de l'Université de Montréal, Canada)
MRI in Radiation Oncology. See what you treat - treat what you see1,2
Juergen Debus (University Hospital Heidelberg, Germany)
Collaboration between Radiology and Radiation Oncology for MR-guided Radiotherapy1
Hersh Chandarana (New York University, New York, NY, USA)
Watching Cancer Develop Multidrug Resistance
Prof. Anwar R. Padhani, MB, BS, FRCP, FRCR et al., Paul Strickland Scanner Centre, Northwood, Middlesex, United Kingdom
Tumor therapy assessment with OncoTreat
Peter Gall, Ph.D., Siemens Healthineers, Erlangen, Germany
MRI in the Radiotherapy Process, Now and in the Future
Mikael Karlsson, Umeå University Hospital, Umeå, Sweden
Did this information help you?
Thank you.
The name "myExam RT Assist" is used starting from software version syngo MR XA50. In former software versions it is called "RT Dot Engine".
syngo.via VB10 and the syngo.via VB10 based software options are currently under development, and not for sale in the U.S., China and other countries. Due to regulatory reasons its future availability cannot be guaranteed. Please contact your local Siemens Healthineers organization for further details.
syngo.via VB10 and the syngo.via based software options are currently under development; not for sale in the U.S. and other countries. Future availability cannot be guaranteed.
The herein illustrated statements made by Siemens’ customers and physicians are based on their own and discrete opinion and do not reflect Siemens Healthineers' opinion. Siemens Healthineers dissociates from the content and Siemens Healthineers does not intend to promote the content of the statement as true, state of the art or as Siemens Healthineers opinion. The Siemens Healthineers' customers and physicians have not made these statements due to any financial support or contribution by Siemens Healthineers or due to any other contractual obligation. The distribution of these statements by Siemens Healthineers shall only illustrate the variety of different opinions and approaches regarding MR technology.
